- Tendera M. Epidemiology, treatment, and guidelines for the treatment of heart failure in Europe. Eur Hear J Suppl. 2005;7(Suppl J):J5-J9. doi:10.1093/eurheartj/sui056.
- Chronic heart failure in adults: diagnosis and management. 2018, available at https://www.nice.org.uk/guidance/ng106.
- Ebner N, von Haehling S. Iron deficiency in heart failure: a practical guide. Nutrients. 2013;5(9):3730-9. doi:10.3390/nu5093730.
- Klip IT, Comin-Colet J, Voors A a, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(4):575-582.e3. doi:10.1016/j.ahj.2013.01.017.
- McDonagh TA, et al; Eur Heart J. 2021 Aug 27; doi: 10.1093/eurheartj/ehab368.
- https://www.verywellhealth.com/heart-failure-causes-and-risk-factors-1746181
- https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- Marchi G, Busti F, Vianello A, Girelli D. Anemia and iron deficiency in heart failure: extending evidences from chronic to acute setting. Intern Emerg Med. 2020 Jul 10. doi: 10.1007/s11739-020-02434-9. Epub ahead of print.
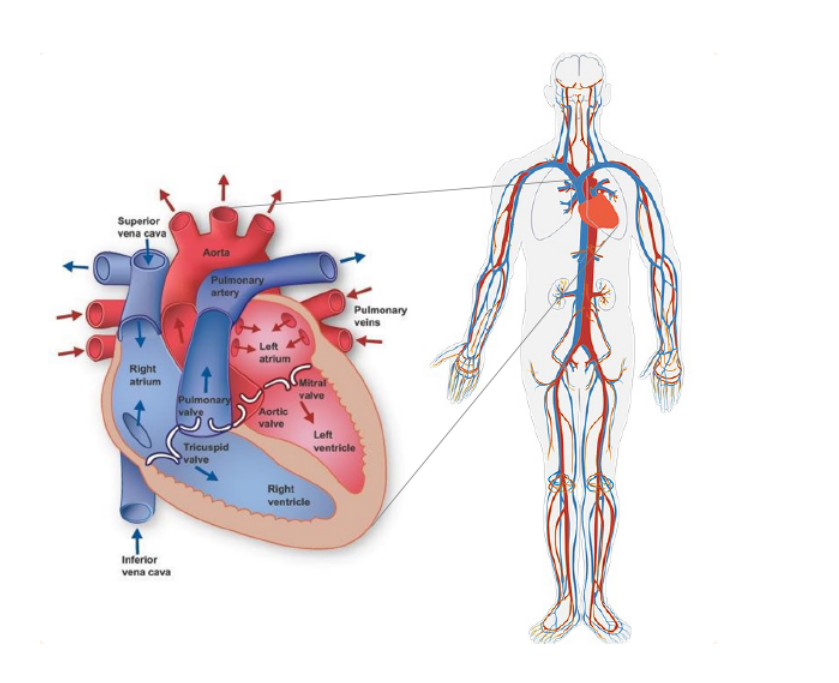
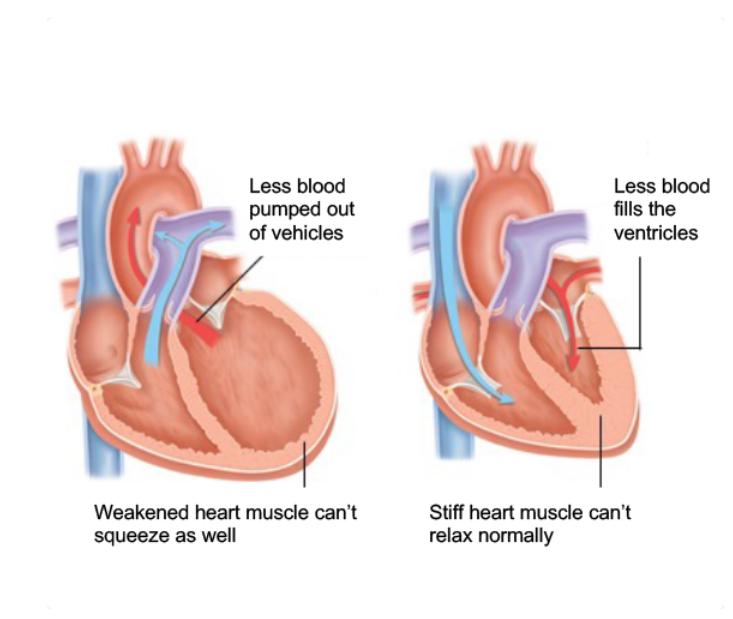
Heart failure means that your heart has been weakened or damaged and can no longer pump all the blood that you need around your body.
Your chronic heart failure may mean you feel exhausted and get out of breath more easily than you used to. These symptoms may be partly due to iron deficiency.
If you have been diagnosed with chronic heart failure you will probably have follow-up appointments with your doctor to check how you are getting on with your heart medication. You can use this opportunity to discuss any other symptoms you are experiencing, or make an extra appointment so that you and your doctor have plenty of time. To help you remember everything you wanted to ask, make notes beforehand. That way you will have all the information the doctor might need. Your iron levels can be checked by a blood test – follow the link to find out more about the blood tests and what the results mean.
Once your doctor has tested your iron levels they can decide which treatment is best for you. This will depend on the level of iron deficiency you have, and could be advice on how to get more iron in your diet and/or recommendations for medication that you can take to improve your iron levels. More information on the different treatment options and how to get the most iron from your diet can be found by following the link.
Heart failure means that your heart has been weakened or damaged and can no longer pump all the blood that you need around your body.
Your chronic heart failure may mean you feel exhausted and get out of breath more easily than you used to. These symptoms may be partly due to iron deficiency.
If you have been diagnosed with chronic heart failure you will probably have follow-up appointments with your doctor to check how you are getting on with your heart medication. You can use this opportunity to discuss any other symptoms you are experiencing, or make an extra appointment so that you and your doctor have plenty of time. To help you remember everything you wanted to ask, make notes beforehand. That way you will have all the information the doctor might need. Your iron levels can be checked by a blood test – follow the link to find out more about the blood tests and what the results mean.
Once your doctor has tested your iron levels they can decide which treatment is best for you. This will depend on the level of iron deficiency you have, and could be advice on how to get more iron in your diet and/or recommendations for medication that you can take to improve your iron levels. More information on the different treatment options and how to get the most iron from your diet can be found by following the link.